Patients come to us time and time again..
“My neck and shoulders are just constantly tight and nothing I do helps”
Usually these people have seen multiple Chiros and Physios and some “get it” better than others… It’s not really until we start to dive deeper and ask a simple question.. “Did you injure your neck? Or did this develop gradually?” most people say, “...it developed gradually”.
When a problem is not traumatic, and is behavioural, we need to look at why YOUR behaviour creates pain, rather than trying to find a ‘fix’ or a solution in the clinic.
The solution is already in your hands
Here are 3 main things we find as significant contributors to this constant neck and shoulder tightness:
Prolonged positions. Even if you have 'good posture', not moving for extended periods of time is not something to be proud of. Let's put it this way... Would you drink stagnant water? Conceptually we need to think of our bodies the same way; constantly moving, dynamic and fresh, like a flowing stream of water.
Staying stuck in a position also forces some muscles connected to your neck and shoulders to over work to maintain an upright position, especially if you're also in a seated position all the time. You don't have the support of your hips helping you out and you're mainly looking in one direction.
Not only that, but ‘Computer Vision Syndrome’ is something that people start to experience because of prolonged positioning, but also adding the strain of constant eye focus on the screen of your computer. So, a combination of not putting demands on your body along with an overuse of only a few muscles to keep your position constant and glaring at a screen can result in always feeling 'tight' in the shoulders and neck.
Prolonged fight or flight. Have you ever been told that you "need to reduce your stress"? And how likely is that? I'd say not very.
Stress is a normal part of our lives. Without it, we're all comfortable. It really does come down to getting to know yourself well enough to know how to manage that stress that's incoming… but even the best of us aren't perfect and we can creep into a chronically stressed state... and that's one issue that leads to a range of deleterious health effects and with respect to tightness in the neck - an increased sensitivity to pain signals and an upregulation of perceived environmental threat.
Sensitivity to pain signals - anything that was just a little bit tight, can start to feel painful. Mechanically it will 'feel' tighter but that's often because of the chronically stressful state rather than what's happening mechanically.
Upregulating perceived environmental threats - our nervous systems are geared for survival - in nature, we're smart, but we're not exactly hunters.... So really, if we hear something loud, or see something moving fast, we have reflexes that tighten our neck and shoulders so we can react quickly...
This is the same stress response we are eliciting when sitting at your computer, so your neck and shoulders are tightening up in preparation to fight or flight... That's why stretching them out doesn't really work - you need to change your state and change your environment to help you reset.
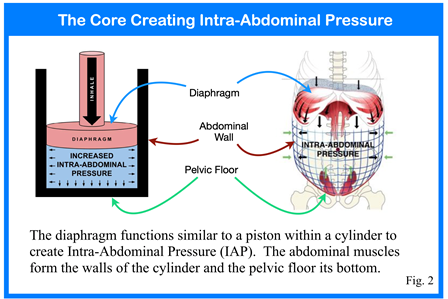
Poor breathing patterns. Let's combine stress with prolonged positioning, now let's just slouch a little too - now there is no room for your diaphragm to lower.... but you still have to get the air in - so you breathe through your chest by elevating your shoulders.
The way you breath tells your nervous system what state it's in, so when you combine everything we've talked about so far - you can see that it's a vicious cycle. Remember, your shoulders and neck are busy sustaining your position all day, but the added extra is that we take around 25,000 breaths a day, so if you're raising your shoulders to do so, now your shoulders and neck are working hard to help you breath AND sustain your position WHILST your in a stressful state...
I hope that explains why your neck and shoulders feel tight all the time!
We’re here for you, providing Chiropractic and Physiotherapy in 4 locations in Sydney - Norwest, Bondi Junction, Brookvale and Penrith and our brand new location in Virginia QLD - so hopefully we’re close to you or someone you know.
Whether it’s neck pain, headaches, shoulder pain or just need some tips, we can help.. And if you’re not sure, feel free to reach out via email admin@balancehp.com.au or give us a call on (02) 9899 5512.